Laryngopharyngeal Reflux (LPR) and how to manage it
You have probably been directed to this blog because your ENT specialist has identified laryngopharyngeal reflux as a cause of your ENT symptoms. Laryngopharyngeal reflux (or LPR for short) is an extremely common condition that affects many of the patients that we see in our ENT Clinic. The symptoms that this condition may cause include hoarseness, a sore throat, a sensation of something stuck in the throat (a symptom we call “globus”), a chronic dry cough, and occasionally a persistent sense of phlegm in the throat or a postnasal drip.
Typically, LPR occurs at night when the patient is lying in a horizontal position. Stomach contents are more likely to spill into the oesophagus and larynx causing irritation. Symptoms are therefore more common at night or in the morning. Patients describe waking up with a sore throat, a hoarse or croaky voice, and a sensation of phlegm. A tendency to clear the throat often exists this can lead to embarrassment in the workplace, or annoy colleagues and other family members. Indeed, one of my patients was brought to see me by his wife who was driven to despair by his throat-clearing habit!
What causes LPR?
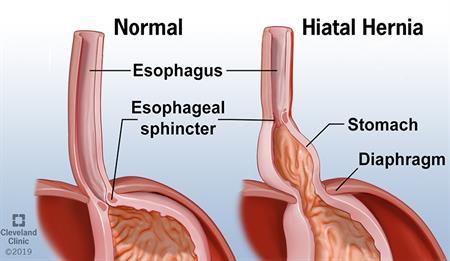
There are a variety of factors that predispose an individual to LPR. Some factors that directly related to the anatomy of the stomach and oesophagus. A hiatus hernia is one common condition that increases the risk of LPR. The hernia disrupts the lower oesophageal sphincter which is a valve that keeps stomach contents within the stomach.
Obesity – especially truncal obesity – predisposes to LPR. A sedentary life style and smoking are also contributory factors. Patients who eat irregularly, or have large dinners late at night often have LPR. Ideally, dinners should be small and light and one shouldn’t lie down for at least 3-4 hours after dinner. In fact, a brisk walk after dinner has much to commend it.
Caffeine relaxes the lower oesophageal sphincter and causes LPR. Caffeine is not only present in coffee! Green tea and sodas contained a lot of caffeine. Many of my patients with LPR think green tea is a caffeine-free drink that helps with weight loss, and so imbibes large volumes during the day.

The other foods and beverages that stimulate acid reflux are spicy foods, curries, citrus fruits, and certain alcoholic drinks. It is noteworthy that beers and wines stimulate acid production more than gin, vodka, and tequila. So if you had to have a drink and suffer LPR, go for a gin and tonic!
How is LPR diagnosed?
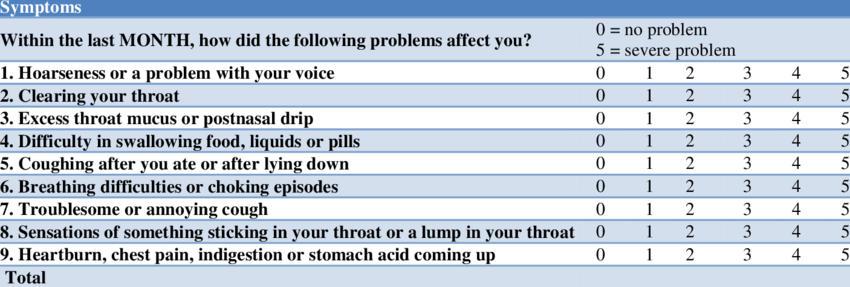
LPR can be extremely difficult to diagnose. As specialists, we rely heavily on the history that the patient gives. The reflux symptom index is a validated questionnaire that is often used to assess the likelihood of LPR. I have reproduced it below. A total score of more than 13 is widely regarded as positive for a diagnosis of LPR.
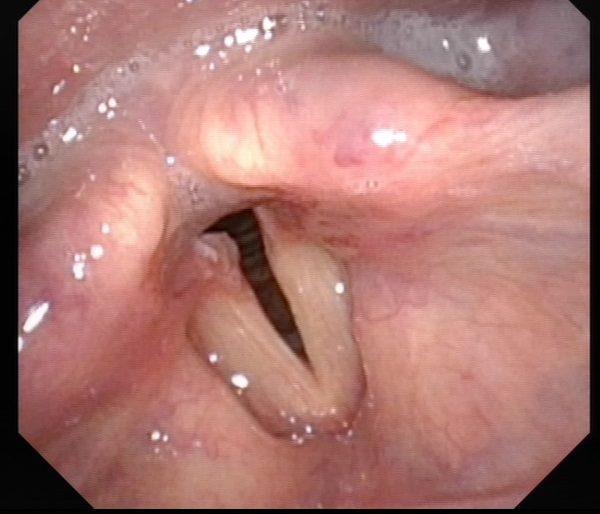
As ENTs, we also rely heavily upon clinical examination of the throat. We would normally recommend an endoscopy of the upper airway by inserting a flexible scope through your nose. This investigation allows us to exclude other conditions that may mimic the symptoms of LPR. In the absence of other pathology, there are features that allude to the diagnosis of LPR. These include redness of the voice box, thickening of the back of the vocal folds, excess phlegm or thickened laryngeal secretions, and rarely a contact ulcer or benign growth (granuloma) of the vocal processes.
The gold standard in diagnosing LPR is to measure the pH at the level of the larynx over a 24 hours period. This technology will soon be available in The ENT Clinic.
Laryngopharyngeal Reflux (LPR) and how to manage it
I can’t possibly have LPR, I don’t have any heartburn
Restech pH Monitoring System
Restech pH Monitoring SystemThis is a common protestation by most patients when we diagnose them with LPR. Many patients with LPR will not have symptoms of heartburn. Heartburn or dyspepsia is a feature of gastro-oesophageal reflux disease or GERD. The two may or may not co-exist. The presence of LPR without symptoms of dyspepsia is often described as “silent reflux”
How can I manage LPR?
There are multiple ways in which LPR can be managed. In most cases, we will begin by addressing dietary and lifestyle issues. Eating regular meals and having small dinners which are less oily and spicy is important. Not lying down too soon after dinner will give time for the stomach to digest the food and empty itself into the small intestine. Avoiding beer and wines in excess at night is important. I usually counsel patients to limit themselves to a cup of coffee/ tea/soda a day. Mints, chocolates and creamy foods are also best avoided. Smoking tobacco should be ceased or reduced.
There are certain interventions that have limited evidence of efficacy but are growing in popularity. These include the consumption of apple cider vinegar before a meal and drinking alkaline water.
Some patients will need medication to help with their reflux. We usually employ alginates such as Gaviscon to help line the oesophagus and proton-pump inhibitors (PPIs) such as Nexium, Pariet, or Dexilant to suppress the production of acid by the parietal cells in the gastric lining. In recent years, a new class of acid-suppressing drugs has come onto the market. These potassium competitive acid blockers (PCABs) such as Vocinti have a much stronger acid-suppressing effect and do not need to be consumed before meals, unlike most conventional PPIs.
The general prognosis for LPR is good. With simple measures and short periods on medication, most people go into good long-term remission.
END
Share this blog via:
