Allergen immunotherapy for allergic rhinitis

Allergies are extremely common and often manifest in young children and adults. Allergies to inhalant allergens such as house dust mites, animal dander, and pollens often present as sneezing, itching, a runny nose, and breathing difficulties. When allergies affect the nose, the patients are said to have allergic rhinitis. When the main manifestations are breathing difficulties, coughing, or wheezing it is often called atopic asthma.
Allergies are fundamentally due to an ‘abnormal’ immune system reaction to common and essentially harmless proteins in the atmosphere. The immune system is principally meant to attack harmful viruses and bacteria. However, in allergic patients, the immune system starts to ‘react’ to elements in the environment such as dust mite proteins.
Diagnosing allergies
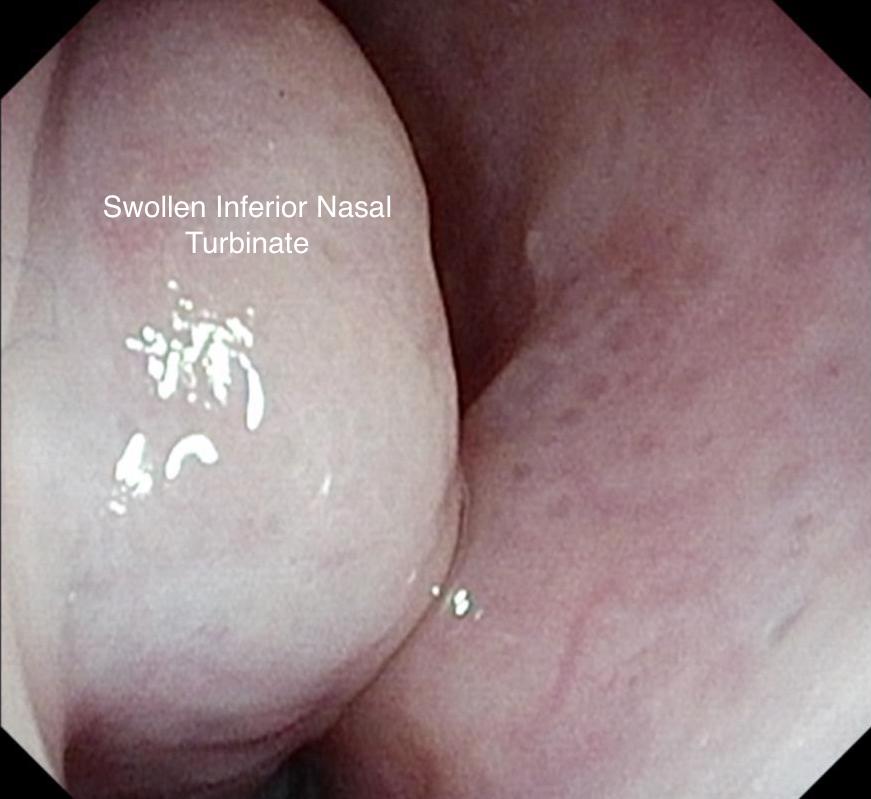
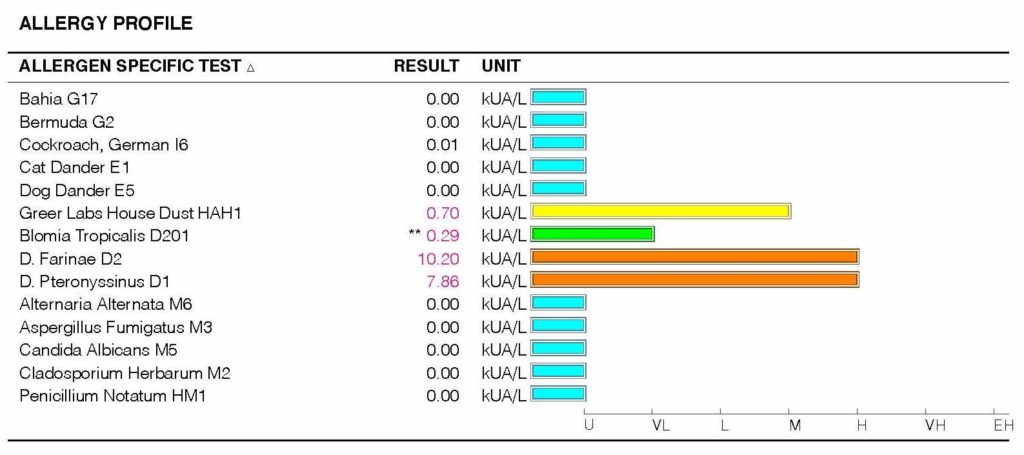
Doctors diagnose allergies by making a clinical assessment of a patient’s respiratory system. This includes taking a history of the symptoms the patient suffers and examining their nasal airway and lung. ENT specialists will make the diagnosis by examining the nose by nasal endoscopy. Allergies are then confirmed by either skin prick testing or blood tests. These blood tests measure the level of an antibody in the blood called Immunoglobulin E (IgE) that is raised in allergies. Specific IgE testing using the ImmunoCap assay can identify the specific allergy that may be responsible for the patients’ allergies. Another test we frequently employ is the Phadiatop test which is highly sensitive for inhalant allergies.
Treating allergies – the conventional way
Allergic rhinitis is treated by educating the patient about their allergies and reducing the ‘allergen load’ in their environment. This is the keystone of allergy management but is often forgotten! Children who have house dust mite allergies should have their soft toys in bed reduced or taken away! Bed linen should be hot washed at 60 degrees Celsius. Carpets and rugs should be removed and books and toys that accumulated dust taken away from the bedroom.
The other strategies employed by primary care physicians are the use of antihistamines and nasal steroid sprays. Antihistamines counter the histamines released by the immune cascade that is triggered by an allergen. So they really mop up the histamine released in the nose and lung. They are generally inferior to nasal steroid sprays in the treatment of allergic rhinitis. Nasal steroids work at the intracellular level and reduce the release of histamines and other inflammatory chemicals.
Treating allergies with Allergen Immunotherapy
Allergen immunotherapy has been around since 1911 – so it is not a new intervention for allergies. It was first used to treat hayfever allergy at St Mary’s Hospital, London. In recent years, there has been a growth in our knowledge of the use of immunotherapy in clinical practice. Guidelines from various expert bodies such as the European Academy for Allergy and Clinical Immunology (EAACI) and robust safety and efficacy data from the European Medicines Agency (EMA) and US Food and Drug Administration (USFDA) has led to their common use in ENT.

What is allergen immunotherapy?
Allergen immunotherapy involves the regular administration of an allergen extract on a daily basis for several years. This causes the immune system to switch off the allergic response to the allergen. Some would say it is like a vaccine and in many ways this analogy is valid. There are two ways of administering allergen immunotherapy:
- Subcutaneous Immunotherapy (SCIT). This involves regular injections of the allergen extract. These injections are delivered by a fine needle into the skin. Initially these injections are weekly and the dose of allergen increaseed sequentially. Eventually, the maintenance dose is given on a monthly basis
- Sublingual immunotherapy (SLIT). This involves the daily use of drops or dissolving tablets that are placed in the mouth (usually under the tongue where absorption is optimal). This is best done in the morning before food. The medicine is kept in the mouth for 2 minutes and then swallowed. Food is then avoided for 15 minutes. At The ENT Clinic, we offer two types of sublingual immunotherapy. The first is OralTek (a liquid) which is ideal for children and the second is Acarizax (a tablet specifically for dust mites) which is more suitable for older children and adults. Sublingual immunotherapy has been used since the 1980s and is particularly good for inhalant allergies (e.g. grass pollen, house dust mites)
What are the side effects of allergen immunotherapy?
Allergen immunotherapy can stimulate all the same reactions that allergies cause in patients. So it is common to have itching or burning of the mouth, lip swelling, or even heartburn when you start this treatment. We often advise using antihistamines to ameliorate some of these side effects. After some time, the side effects of this treatment wanes and most patients tolerate this medication well. There are few long-term side effects of allergen immunotherapy. One rare symptom is heartburn due to a condition called eosinophilic oesophagitis (EoE). Should this occur, most patients will be advised to stop treatment
How effective is allergen immunotherapy?
Allergen immunotherapy is highly effective in reducing the symptoms of allergies and the dependence on medications such as nasal sprays and antihistamines. It also disrupts the “allergic march” where children with allergic rhinitis go on to develop asthma around the age of 7 years. Most studies show that over 80% of patients will derive benefit
In 2010, a fairly robust analysis of 49 randomised trials comparing 2333 patients receiving sublingual immunotherapy with 2256 patients receiving a placebo showed a statistically significant improvement in symptoms and reduction in the use of medicines to treat symptoms of allergic rhinitis. None of these 49 trials reported any serious side effects from sublingual immunotherapy.
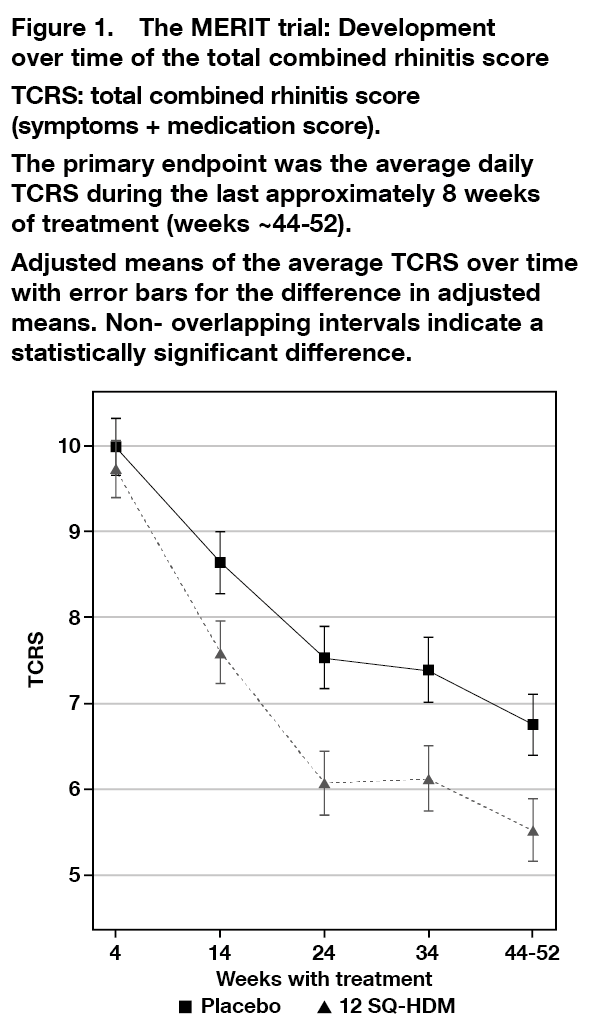
One of the common preparations we use at The ENT Clinic is Acarizax by Abbott. This contains the extract of two common dust mites – Dermatophagoides pteronyssinus and Dermatophagoides farinae – but has a bystander effect by promoting desensitisation to Blomia Tropicalis too. The diagram below from the Merit Trial shows that benefits of treatment with Acarizax are noticed within 14 weeks of treatment
How long do the beneficial effects last after treatment is discontinued?
The evidence shows that the immunological and clinical benefits of immunotherapy last for at least 3 years following cessation of treatment
How much does allergen immunotherapy cost?
At The ENT Clinic, our prices for the two most commonly used are as follows (prices are accurate as of 1 July 2021):
- Acarizax – SGD$200 per month before GST
- OralTek – SGD$470 per quarter before GST
How do we start treatment?
Most patients are advised to optimise the control of their allergic rhinitis with nasal steroid sprays and antihistamines before commencing immunotherapy. Regular consumption of antihistamines for a week before immunotherapy is initiated helps reduce the side effects and ensure good treatment compliance.
For Acarizax, most patients may be asked to remain in the clinic for 15-30 minute to ensure so severe reactions or anaphylaxis is encountered when the first dose is given.
What is the treatment duration?
Most patients will require 3-5 years of treatment to ensure good long term remission of allergies
How do I know treatment is effective?
The best measure of successful treatment is the reduction in symptoms and the need for nasal sprays and antihistamines. Many patients ask if there is a way to test if treatment is beneficial. Unfortunately, blood tests to measure the levels of specific IgE antibodies are of little use. These antibodies will remain present. Assays to measure the level of blocking IgG antibodies – which effectively inactivate the specific IgEs – are not routinely available in clinical practice.
One reasonable approach to assess the efficacy of allergen immunotherapy is to perform a skin prick test. There is recent evidence to suggest that reduction in grade of skin prick test correlates well with efficacy particularly in children with a low total IgE level or a high specific: total IgE ratio (see https://doi.org/10.1080/21645515.2018.1482171)
Summary points
- Allergen immunotherapy is a safe and well established treatment for switching off allergies
- It is highly effective for inhalant allergens
- Compliance with 3-5 years of treatment is important
- The effect of immunotherapy last for at least 3 years following cessation of treatment
If you have any queries about allergen immunotherapy, feel free to contact us to a schedule a consultation.
Dr Jeeve Kanagalingam for The ENT Clinic
Share this blog via:
